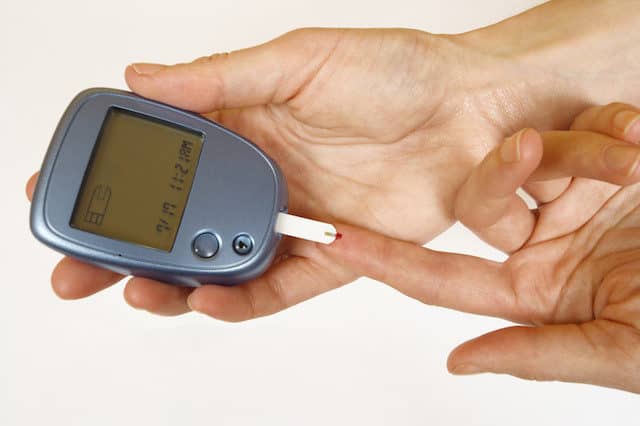
A new report out of the United Kingdom says that a holistic care program delivered mostly by nurses can result in shorter stays at the hospital for diabetes patients. The study was led by Gerry Rayman from Ipswich Hospital. The program is called Diabetes Inpatient Care and Education (DICE). It was set up to use new technologies and education methods to find the diabetes patients that needed specialists the most.
A new report out of the United Kingdom says that a holistic care program delivered mostly by nurses can result in shorter stays at the hospital for diabetes patients. The study was led by Gerry Rayman from Ipswich Hospital. The program is called Diabetes Inpatient Care and Education (DICE). It was set up to use new technologies and education methods to find the diabetes patients that needed specialists the most.
The researchers evaluated the holistic program by judging its impact on the length of each patient’s stay, the diabetes mortality rate in the hospital, and how many people were readmitted to Ipswich Hospital over an eight year period.
The Study
 Before the holistic DICE program was used, 2,337 patients with diabetes were admitted. This number remained roughly the same in the six months after DICE was brought in. However, the use of DICE also gave some encouraging statistics, which Rayman and the other researchers included in their report in Diabetic Medicine. For example, the average length of stay for each diabetic patient went from 7.5 days down to 6.7 days. They also took the study one step further and made adjustments in those numbers for variables like age, sex, race, and type of admission. After the adjustment, the results were even more encouraging. The average hospital stay went down more than 15%.
Before the holistic DICE program was used, 2,337 patients with diabetes were admitted. This number remained roughly the same in the six months after DICE was brought in. However, the use of DICE also gave some encouraging statistics, which Rayman and the other researchers included in their report in Diabetic Medicine. For example, the average length of stay for each diabetic patient went from 7.5 days down to 6.7 days. They also took the study one step further and made adjustments in those numbers for variables like age, sex, race, and type of admission. After the adjustment, the results were even more encouraging. The average hospital stay went down more than 15%.
Same Study, a Different Approach
The research team then repeated their analysis, but with statistics from the entire eight year period from 2008 to 2016. When compared over a longer period, the introduction of DICE to the hospital still showed a decrease in time of hospital stay in diabetic patients. The team also noted that DICE did not have this similar effect on patients without a diabetic condition.
Other Findings
Another significant finding for Rayman and his colleagues was that deaths among diabetic patients fell drastically. Mortality saw a nearly 40% reduction among diabetics that had been admitted to the hospital. DICE also caused a 20% drop in deaths among the non-diabetic patients. However, these results were not consistent when compared over the full eight year period. Also, over the longer period, readmission rates were higher for patients with diabetes.
Rayman said his biggest conclusion is that a well staffed inpatient team can lead to a long term reduction for the length of stay for diabetic patients. This is important because it means that patients will have to spend less on their healthcare. Rayman also said its important to use the longer term analysis in evaluating these sorts of programs. Because so many different factors can influence a patient’s hospital stay and outcomes, the longer term study is often the most important data.