According to a study that appeared in The Journal of Nuclear Medicine, scientists at Bristol-Meyers Squibb (BMS) are developing a new way for physicians to determine how cancer patients might respond to PD-1 (programmed cell death protein 1) and PD-L1 (programmed death-ligand 1) targeted treatments. Previously, the only way to predict that outcome was through an invasive biopsy procedure that took a while to get results. Researchers have now developed an approach that will help scientists to visualize the PD-L1 content of tumors using a simple, non-invasive positron emission tomography (PET) scan.
The Need for PD-1 and PD L-1 Targeted Therapies
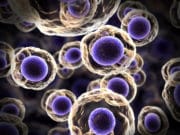
 In a normally functioning immune system, the body maintains a balance between eliminating infections or cancers and making sure that it doesn’t begin to attack itself. PD-1 receptors play a crucial role in regulating this process through immune checkpoints: when PD-1 binds to its ligand, PD-L1, it suppresses T-cell inflammatory activity, down-regulating the immune system and preventing the development of chronic autoimmune diseases. However, this interaction between PD-1 and PDL-1, known as a “checkpoint pathway,” can also stop the immune system from destroying cancer cells.
In a normally functioning immune system, the body maintains a balance between eliminating infections or cancers and making sure that it doesn’t begin to attack itself. PD-1 receptors play a crucial role in regulating this process through immune checkpoints: when PD-1 binds to its ligand, PD-L1, it suppresses T-cell inflammatory activity, down-regulating the immune system and preventing the development of chronic autoimmune diseases. However, this interaction between PD-1 and PDL-1, known as a “checkpoint pathway,” can also stop the immune system from destroying cancer cells.
When T-cells travel to the tumor’s location and kill the cancerous cells, the tumor can escape the body’s natural immune response by using its own high levels of PD-L1 to bind to PD-1 on T-cells and deactivate them. Because tumors that have a high expression of PD-L1 are oftentimes associated with poor treatment outcomes, scientists believe that the increase of PD-L1 is what allows the tumor to escape the body’s immune response. Scientists have thus created certain antibodies “directed against the PD-1/PD-L1 pathway” which help to treat several kinds of cancer.
How PET Scans Identify PD-L1 in Tumors
 The new PET scan method will offer a way for scientists to see which tumors contain PD-L1, which will indicate that they should respond positively to immune checkpoint inhibitor therapies. BMS, the first institution to research this method, used a “radioligand,” a kind of radioactive biochemical material, to find the tumors with PD-L1. They combined radioactive fluorine-18 (18F), commonly used as a tracer in PET scans, with a protein called Adnectin, to create an image tracer called 18F-BMS-986192. The researchers tested this tracer in mice with tumors, and they tested its distribution, binding, and dosage in a healthy monkey, determining that it’s safe to use in humans. The study reported that 18F-BMS-986192 bound to tumors that contained PD-L1, which allowed researchers to use the PET imaging to visualize the PD-L1 in the mice.
The new PET scan method will offer a way for scientists to see which tumors contain PD-L1, which will indicate that they should respond positively to immune checkpoint inhibitor therapies. BMS, the first institution to research this method, used a “radioligand,” a kind of radioactive biochemical material, to find the tumors with PD-L1. They combined radioactive fluorine-18 (18F), commonly used as a tracer in PET scans, with a protein called Adnectin, to create an image tracer called 18F-BMS-986192. The researchers tested this tracer in mice with tumors, and they tested its distribution, binding, and dosage in a healthy monkey, determining that it’s safe to use in humans. The study reported that 18F-BMS-986192 bound to tumors that contained PD-L1, which allowed researchers to use the PET imaging to visualize the PD-L1 in the mice.
Benefits of the PET Scan Method for Cancer Patients
This new approach not only eliminates the need for an invasive biopsy, but also speeds up the process of determining the kinds of therapies that will be most effective for a particular patient. In a press release, David J. Donelly, senior research investigator at BMS Research and Development, explained that the technique “represents an opportunity for physicians to non-invasively assess all of a patient’s tumors for PD-L1 expression with a single PET scan and timely readout.” He added, “This may help guide treatment decisions and assess treatment response, to help identity the right treatment for the right patient at the right time and right dose.”
Researchers at BMS indicated that clinical trials with 18F-BMS-986192 are currently being conducted in order to evaluate PD-L1 expression in in human tumors.























An exosome quantitative blood or urine test which would count the number of cancer cell exosomes carrying the same PD1-PDL1 biomarkers as found on cancer cells membranes would be a much more effective monitor than a PET scan and would hopefully be able to see these cancer cell exosomes years before a PET scan and it would be much less invasive and cheaper – which is probably why were don’t see articles like this on exosomes – less money to be made for the health care economy.