What is the future of cancer immunotherapy methods? Let’s have a look…
One method is through the up-regulation of immune checkpoint molecules, such as programmed death 1 (PD-1) and its ligand (PDL1), which deactivate T cells, a main attacker of tumor cells. … Unlike chemotherapy, which acts directly on the tumor, immunotherapy acts on the immune system, which then acts on the tumor.
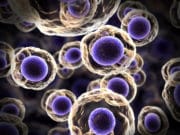
The latest FDA-approved cancer immunotherapies have included multiple immune checkpoint inhibitors. To prevent inappropriate destruction of the host, the human immune system is composed of multiple checks and balances called immune checkpoints. These checkpoints consist of pathways that, when triggered, will deactivate the attacking immune cell.
Unfortunately, many cancers have devised ways of manipulating this system. One method is through the upregulation of immune checkpoint molecules, such as programmed death 1 (PD-1) and its ligand (PDL1), which deactivate T cells, a main attacker of tumor cells. Checkpoint inhibitors that block the activation of these molecules, such as anti-PD-1 or PDL1 antibodies, have shown promise in the clinic, with multiple drugs already receiving FDA approval for the treatment of melanoma and lung cancer.
Unlike chemotherapy, which acts directly on the tumor, immunotherapy acts on the immune system, which then acts on the tumor. This takes time. And if the treatment isn’t effective, the administration of immunotherapy can result in wasted time—time during which a patient could have received another treatment. Thus, it would be advantageous if a predictive test—in particular, a speedy, noninvasive one—could be used to predict immunotherapy efficacy early in treatment.
To that end, my colleagues and I are working to develop such a test, based on patients’ personal T-cell receptor repertoires (TCRRs).
Every person has a unique TCRR, one that’s constantly changing in response to immune stimuli. For example, if a person gets the flu vaccine, the T-cell receptors responsible for recognizing flu antigens will become activated and those T cells will expand. The person now has a new TCRR, which consists of more flu-recognizing T-cell receptors. This is called clonal expansion.
In our lab and elsewhere, researchers have recently begun exploring changes in clonal expansion in response to cancer immunotherapy, especially those related to immune checkpoint inhibitors. The prevailing thought is: if blocking immune checkpoints leads to changes in a person’s immune system, T cells with unique receptors will be activated, resulting in increased clonal expansion.
In one recent study, investigators from the University of California, Los Angeles (UCLA), and their colleagues tested the effect of an anti-PD-1 on TCRRs in melanoma patients. To assess TCRR, the researchers isolated tumor samples before and after treatment, then sequenced the T-cell receptor gene. Because every T-cell receptor is made antigen-specific through genetic recombination, sequencing enabled the researchers to identify the unique clones and, therefore, each patient’s TCRR. They discovered that patients with clonal expansion showed a much greater response to anti-PD-1 treatment.
Separately, the UCLA team showed that treatment with another checkpoint inhibitor—a monoclonal antibody against CTLA4 (anti-CTLA4)—resulted in an increase in clonal expansion in melanoma patients’ peripheral blood mononuclear cells (PBMCs). PBMCs are isolated from blood, paving the way for noninvasive screens to analyze a patient’s TCRR.
Together, these studies have demonstrated that assessing patients’ TCRRs could eventually help researchers predict the efficacy of cancer immunotherapy treatments much earlier, allowing for the more effective use of these treatments in the fight against cancer.
Monoclonal antibodies are expensive. Precision medicine combines a complete DNA sequence and targeted drugs (new and old drugs) to treat cancer (being used by select hospitals in the country).
Until recently, most immunotherapeutic approaches used to fight cancer were ineffective, counteracted by the tumour’s ability to evade immune attack. However, extensive research has improved our understanding of tumour immunology and enabled the development of novel treatments that can harness the patient’s immune system and prevent immune escape. Over the last few years, through numerous clinical trials and real-world experience, we have accumulated a large amount of evidence regarding the potential for long-term survival with immunotherapy agents in various types of malignancy. The results of these studies have also highlighted a number of recurring observations with immuno-oncology agents, including their potential for clinical application across a broad patient population and for both conventional and unconventional response patterns. Furthermore, given the numerous immune checkpoints that exist and the multiple mechanisms used by tumours to escape the immune system, targeting distinct checkpoint pathways using combination approaches is an attractive therapeutic strategy with the potential to further enhance the anti-tumour immune response.