It may be just the start… BUT cancer patient’s lives are being saved by immunotherapy which is genetically engineered immune cells that fight cancer

The best part is that it could be available to the public in 1-2 years
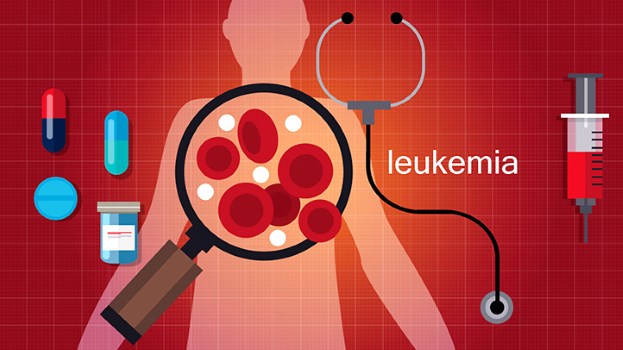
The doctors saw a little girl with leukemia while looking at Layla Richards. The cancer thrived even though she’d had gone through chemotherapy and a bone marrow transplant. By last June all you saw was a 12 month old that was desperately ill. At that point her parents were begging… wasn’t there anything?
Actually there was. The vial of genetically altered white blood cells that are designed to hunt and destroy leukemia was sitting in a freezer at the Great Ormond Street Hospital in London, but the hospital didn’t seek permission to test them yet. With the total of four genetic modifications, two of them introduced by the technique of genome editing… they were the most thoroughly engineered cells ever proposed as therapy.
It didn’t take long for a doctor from Great Ormond to get on the phone with Cellectis, a French biotechnology company that is located on the East Side of Manhattan, the company owned the cancer treatment. They devised this method of treatment using a gene-editing method called TALENs, a method of modifying the DNA in living cells. “We got a call. The doctors said, ‘We’ve got a girl who is out of T cells and out of options,’” André Choulika, the CEO of Cellectis, remembers. “They wanted one of the vials made during quality-control testing.”
The doctors wanted to make Layla a “special,” which is a patient who gets the drug outside a clinical trial. The company’s stock and reputations could tank if it failed and even if it was a success, the company might get in trouble with regulators. “It was saving a life versus the chance of bad news,” Choulika says. Since the treatment had only been tried on mice, it was a gamble.
In 2011 Cellectis started developing the treatment after doctors in New York and Philadelphia proclaimed they found a way to take control over the killer cells of the immune system, T cells. With the use of a virus, they had shown that they could take T cells from the bloodstream and add new DNA
instructions to target them at the type of blood cell that goes awry in leukemia. This approach has been
tested in more than 300 patients, often showing spectacular results, complete remission. Now over 10
biotechnology companies and drug firms are working to deliver such a treatment to market.
There may be an even broader applications for the T cells created by Cellectis. The treatments use a
person’s own cells, but in some patients like Layla don’t have enough T cells. This is especially true for
small children. Foreseeing this problem they set out to use gene editing to create a more highly
engineered but simpler “universal” supply of T cells from the blood of donors. The company would still
add new DNA, but also use gene editing to remove the receptor that T cells normally use to find foreign-
looking molecule.
Choulika says, “The T cell has a huge potential for killing. But the thing you can’t do is inject T cells from
Mr. Z into Mr. Y. They’d recognize Mr. Y as ‘non-self’ and start firing off at everything, and the patient
will melt down.” The risk can be mostly eliminated, or so everyone hoped, if the T cells are stripped
down with gene editing, like the cells that were in Great Ormond’s freezer.
It was announced that Layla was cured in November and the press jumped all over this amazingly
heartwarming story, which sent Cellectis’s stock price shoot upward. Within two weeks, drug companies
Pfizer and Servier announce they would purchase rights to the treat for $40 million.
The role of the T cells in her cure remain foggy since many of the details of Layla’s case haven’t been
disclosed. Her recovery put a spotlight on “immune engineering,” which are leading to breakthroughs in
cancer treatment and could also lead to new treatments for HIV and autoimmune diseases.
The human immune system some call nature’s “weapon of mass destruction,” has a dozen major cell
types, including numerous kinds of T cells. Avoiding harming the body’s own tissue for the most part, it
defends against viruses it’s never seen before, and can suppresses cancer even though this isn’t always
the case. The immune system even has a memory… which is the groundwork of all vaccines.
Over 100 years ago American surgeon William Coley injected streptococcal cultures into cancer patients
and witnessed in some cases that the tumors shrank after observing that an unexpected infection could
sometimes make a vanish. Published in 1893, the finding showed the immune system could fight
cancer… But how did it work? Until recently no one knew, and cancer immunotherapy was seen as a
failed concept. Scientist have gradually mapped the molecules that determine how the immune system
interacts with a tumor and over the last few years have allowed drug companies and labs to start
experimenting with the immune system’s behavior.
The most extreme of these proposals is to change the genetic make-up inside T cells. “It’s the perfect
setup,” says Jeffery Bluestone, a researcher at the University of California, San Francisco. “Immune cells
are machines that work pretty well, but we can make them work even better.”
Decades of research has worked out various important details including how T cells distinguish and
attack invaders. When looking closer through a microscope, these cells show animal-like behavior
almost attacking other cells, they crawl, study, then grab and shoot them full of toxic granules. “What’s
exciting is they have the ability to move all around; they’re autonomous. Immune cells talk to other
cells, they deliver poisons, they can change what happens in a microenvironment, they have a memory,
and they make more of themselves. I think of them as little robots,” says Wendell Lim, a synthetic
biologist who is also at UCSF.
 Lim is breaking new ground and has produced some futuristic T cells… The cells deploy their search and
Lim is breaking new ground and has produced some futuristic T cells… The cells deploy their search and
kill behavior if and only if a specific drug is added, this could be used to “turn on” the cells at specific
places and times, which Lim calls “remote control.” Another cell he designed is two-staged… it kills only
if it locates two different markers on a cancer cell, it’s like a dual authentication for the enemy cell. Lim
thinks of it as an “advanced Google search.” This research is critical because T cell targeting is dangerous
and some have been killed in the trial process, so far, easy ways to target only cancer cells are lacking.
Lim founded a startup, Cell Design Labs, to commercialize his engineering ideas.
Not only are the world’s largest drug companies getting involved in the search to expand immune
therapy but also tech firms… Philip Sharp, a biologist at MIT’s Koch Institute for Integrative Cancer
Research and a recipient of the 1993 Nobel Prize in medicine, says that last year Google held two
summits at MIT with top immune oncologists and bioengineers to figure out what parts of the problem
could be “Googlified.” Google paid special attention to new research techniques that can identify cells
from a tumor biopsy immediately, such methods may generate extensive data about what immune
system cells are doing inside a tumor and insight on their influence. Verily, Google’s life science unit,
hasn’t revealed it plans in cancer immunotherapy so far. Jeffrey Hammerbacher, a former Facebook
employee, is developing software to interpret the DNA sequence in a patient’s cancer and anticipate
from it how to boost the response of the killer T cells. He now runs a lab that is part of Mount Sinai, the
hospital and medical school, with 12 programmers spending time researching T cells.
A clinical trial should start this year, patients get a dose of abnormal protein fragments that the software
predicts will train T cells to attack the cancer. Hammerbacher says “What was fun was that what we
submitted to the [U.S. Food and Drug Administration] was not a molecule but an algorithm. It might be
one of the first times the output of a program is the therapy.”
Juno Therapeutics paid $125 million to acquire AbVitro in January. Abvitro, a Boston-area company
specializing in sequencing the DNA inside single T cells, is trying to detect T cells that are active inside
cancer and study their receptors. Hyam Levitsky, Juno’s chief scientist, says an experiment that used to
take seven months now takes seven days and data is piling up: an average experiment generates 100
gigabytes of information. Levitsy says, “A lot of what is happening is technology-driven. The questions
have been there for a while, but there was no way to get at the answers. Now we’re visualizing them
with new technology in ways we never could before.”
Pfizer has recently started engineering T cells, the company had been negotiating with Cellectis well
before the news of Layla’s treatment and no one at Pfizer was even aware that the girl was treated
before it hit the news. John Lin, head of Pfizer’s head of San Francisco biotech unit says, “The publicity
was a big surprise.”
Years of scientific work have resulted in a level of mastery that makes therapeutic products seems
practical according to Lin. He believes the treatments will have a greater impact that go beyond
leukemia and cancer. “We think that this fundamental principle, engineering human cells, could have
broad implications,” says Lin, “and the immune system will be the most convenient vehicle for it,
because they can move and migrate and play such important roles.”
Researchers are already working on autoimmune disorders and infectious disease is also in the sights of
T cell engineers. Edward Berger, a virologist at the National Institutes of Health, is working with T cells
and HIV. “I was totally inspired by the cancer work,” he says. “They cured leukemia, and we’ve borrowed
it from them. The extension of those ideas for engineering the immune system against other things that
ail people is a major front. I think HIV is the best candidate in infectious disease. If you talk to the HIV
community, they are crying for a cure-a treatment that, ideally, you do once and never again.”