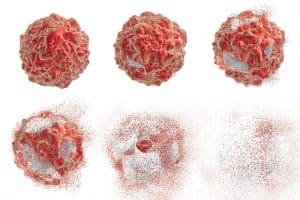
 When cancer develops in the human body, it leads to an uncontrolled growth of a large mass of abnormally-developed cells. In order for the individual to treat the cancer, it’s necessary to kill off those abnormal cells and return the body to its normal conditions. Unfortunately, the process of killing cancer is not an easy one: the individual must endure a sequence of uncomfortable and invasive procedures in order to destroy the cancerous cells, and those procedures might not even be 100% successful.
When cancer develops in the human body, it leads to an uncontrolled growth of a large mass of abnormally-developed cells. In order for the individual to treat the cancer, it’s necessary to kill off those abnormal cells and return the body to its normal conditions. Unfortunately, the process of killing cancer is not an easy one: the individual must endure a sequence of uncomfortable and invasive procedures in order to destroy the cancerous cells, and those procedures might not even be 100% successful.
The common methods that we use to treat cancer today include irradiation, or burning the cancerous cells, chemotherapy, or poisoning the cells, and surgery, which removes the cells from the affected organs, but is only an option when the disease is caught in the early stages.
Although these methods have proved successful in many cases, they are not entirely reliable, as they cannot always guarantee positive results. One of the main reasons that these strong, and sometimes harsh, treatments aren’t successful is that they not only work to destroy cancerous cells, but also to kill off healthy ones, which ultimately creates other health issues in the patient.
This issue is especially detrimental for older patients with already weakened immune systems, as well as for individuals who have other diseases that make it harder for them their bodies to withstand the treatments. The suppression of the immune system in general is one of the most significant consequences of treatments like chemotherapy and radiation.
 Although we still don’t have a 100% surefire way of simply eradicating this deadly disease, scientists have been developing ways for individuals to use their own immune systems to fight cancer, oftentimes combining those methods with traditional treatments. The main reason that we’ve started to incorporate the immune system in the battle to treat cancer is that, simply, it’s the only natural, and the least toxic, tool to fight any kind of disease in the human body.
Although we still don’t have a 100% surefire way of simply eradicating this deadly disease, scientists have been developing ways for individuals to use their own immune systems to fight cancer, oftentimes combining those methods with traditional treatments. The main reason that we’ve started to incorporate the immune system in the battle to treat cancer is that, simply, it’s the only natural, and the least toxic, tool to fight any kind of disease in the human body.
One way that physicians are using the body’s immune system is by using an outside stimulus to “trigger” the patients weakened immune system, which helps it to function at its best. Another method involves injecting parts of the immune system that are artificially created in a lab to contain a higher strength of proteins that are derived from the patient’s specific tumor. This means that when those constructed immune parts enter the body, they can easily recognize the cancerous cells as “foreign” and begin to destroy them. It’s clear, then, that immunotherapy can be seen as a biological therapy that successfully eliminates cancer in a way that’s less toxic than other, more conventional, treatments.
Kinds of Immunotherapy
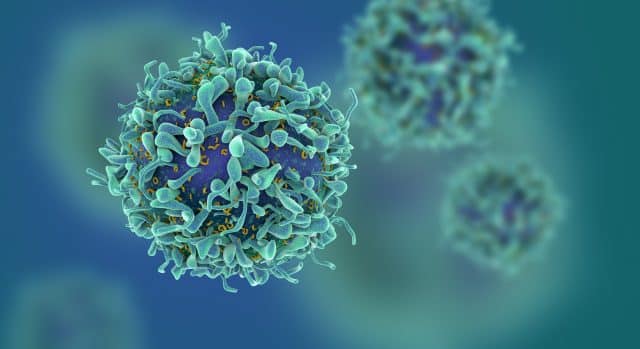
Immunotherapy can be divided into three main classes, which include cell-based, antibody-based, and cytokine-based methods. The therapies involving monoclonal antibodies and cytokines are called passive immunotherapy. When immune cells are adapted to serve the severity of the particular disease and administered to the patient through injections, the therapy is called active immunotherapy.
- Active Immunotherapy: A method that uses two methods, cell-based and vector-based. Cell-based methods involve using a person’s own cells to treat their cancer, and vector-based methods involve using an external path that is genetically created in a lab to give off antigens that are particular to the specific tumor. They are then filled with immune cells and given through an injection.
- Cell-Based Method: A method that acts as a kind of advocate for the patient’s immune system by injecting powerful immune cells directly into the bloodstream. This triggers the immune system as a whole to start fighting, but it also provides the ability to combat cancerous cells specifically.
- Passive Immunotherapy: A method that uses monoclonal (laboratory made) antibodies, as well as cytokines and chemokines to protect against specific targets within the patient’s body. They can be concentrated to work against a specific antigen or found on the surfaces of cancer cells, or a cancer-specific enzyme or protein. Antibodies are one of the most powerful candidates because of their role in adaptive immune responses and also because they are the best at counteracting the harmful effects of antigens. Cytokines and chemokines are great at controlling immune responses, which means that can be used as candidates to eliminate cancerous cells.
- Antibody-Based Therapy: Monoclonal antibodies are created in a laboratory, and they typically involve the use of mouse-models, so the antibodies formed are known as murine antibodies. With the use of mouse models, it’s always possible that the immune system will reject the antibodies and that negative side effects will occur. Chimeric antibodies, which are made up of part mouse and part human antibodies, help to counteract the risk of these negative immune responses. Humanized antibodies are made up mostly of human antibodies, with a few parts being interchanged with their murine counterparts. Human antibodies are made up complete of human antibodies.
Cytokine-Based Therapy: Cytokines are able to modify immune signals, so scientists have begun to use this positive benefit against tumor cells to create cell death. The most common cytokines are Interferons (IFNs) and Interleukins (ILs). The body typically produces Interferons to work against viral infections, but researchers have discovered their efficacy as therapeutic agents that treat cancers, particularly hairy-cell leukemia, AIDS-related Kaposi’s sarcoma, follicular lymphoma, chronic myeloid leukemia, and melanoma. Among the three types of interferons, only IFN type 1 has been shown to be effective at treating cancer.
Research & Development
 Cancer immunotherapy is relatively new in the realm of cancer treatment, so it has many avenues that scientists still need to research and explore. For instance, other kinds of immune cells might be included in the passive immunotherapy methods, since they currently only use antibodies and cytokines. Another possibility that’s being explored for the near future is using T-cells to treat cancer cells by crossbreeding them in the lab with tumor antigens. There is also the possibility of blocking immune checkpoints inside the body, which are often used by tumor cells to escape immunosurveillance.
Cancer immunotherapy is relatively new in the realm of cancer treatment, so it has many avenues that scientists still need to research and explore. For instance, other kinds of immune cells might be included in the passive immunotherapy methods, since they currently only use antibodies and cytokines. Another possibility that’s being explored for the near future is using T-cells to treat cancer cells by crossbreeding them in the lab with tumor antigens. There is also the possibility of blocking immune checkpoints inside the body, which are often used by tumor cells to escape immunosurveillance.